Nearly half of all children in our state – 1.2 million children – rely on Medicaid and NC Health Choice for their health care. These programs are key to ensuring that North Carolina’s kids get the coverage and care they need to stay on track. Unfortunately, these two programs don’t provide children with the same level of care. Starting at age six, some children in the state are moved from Medicaid to NC Health Choice, thereby losing some of the vital coverage Medicaid provides. This loss can be particularly tough on children with special health care needs. Merging the two insurance programs will reduce administrative overhead, and ensure that every child in North Carolina gets the care they need to thrive.
Why does NC have two separate programs?
NC Health Choice (also known as the Children’s Health Insurance Program or CHIP) was implemented in North Carolina in 1998 as a separate, although similar program to children’s Medicaid. Each state has the option to cover CHIP participants within the Medicaid program, create a separate CHIP program, or establish a combination program. Twenty-one states have successfully merged CHIP with Medicaid, but North Carolina has only merged the two programs for children under age six.
Once children enrolled in NC Health Choice turn six, they are at risk of losing access to high-quality, specialized services as well as sustained comprehensive care. Approximately 114,000 children enrolled in NC Health Choice do not have access to the same comprehensive services or other benefits afforded under Medicaid. This can include things like therapies that require frequent visits, or transportation to routine medical care.
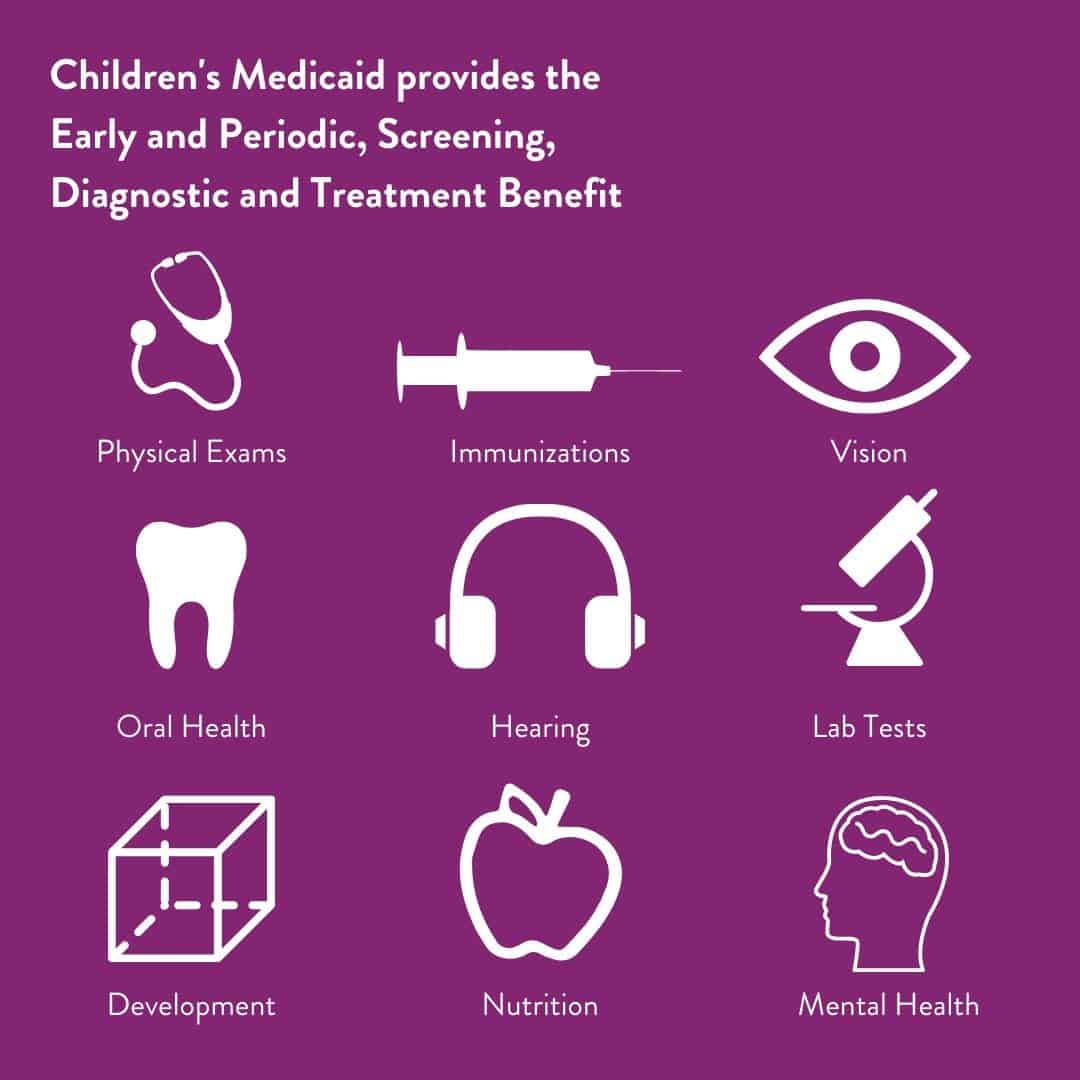
EPSDT is a Cornerstone of Children’s Care
Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) is a fundamental component of Medicaid that guarantees that each child will have access to “all medically necessary care.” EPSDT allows doctors to ensure children are able to get the specific recommended care they need. This is particularly important for children with special health care needs. Unfortunately, the EPSDT benefit is denied to children on NC Health Choice. This can place limits on necessary services. For example, without the EPSDT benefit, children may not be able to get the prescribed number of physical therapy visits per week, or the specific medical device that will help them participate fully at school.
Reducing the Burden on Families
In addition to ensuring children’s health and well-being, a merger of NC Health Choice and Medicaid will decrease red tape for families. Parents with children enrolled in two different programs are often faced with the confusion of children moving from one program to the other, having different therapies or providers available to different children, or confusion at their health care provider about what is covered.
Erica Banks, a member of NC Child’s Parent Advisory Council, has two children who have been covered by both Medicaid and NC Health Choice. “The mailed information is confusing and there is a lack of consistency in the verbiage. One child is on Medicaid, but the other is on Health Choice. Sometimes I have to call and ask if we qualify for certain services – I’m not always sure if it relates to us,” Banks said.
Cost and Administrative Savings
Two programs serving essentially the same population creates administrative duplication for the state. Combining the programs now would simplify administrative management within NC DHHS, reducing barriers to the state’s transformation to Medicaid managed care.
Children served by NC Health Choice make up a small fraction of the children and families served by Medicaid, representing about 7% of those covered. As a result, any cost increase associated with a small uptick in Medicaid enrollment is likely to be offset by administrative savings. Merging NC Health Choice and Medicaid will simplify program management, while returning greater program quality to taxpayers and families.
When children get the care they need, they are better able to grow up healthy and thriving. With Medicaid transformation happening now, this is an important time for elected officials to ensure that all North Carolina children, especially those with special health care needs, are covered and cared for.